Personal Stories
Cheryl’s Story
My Dad – Jim – had experienced and recovered from laryngeal, kidney and bladder cancer over a period of 20 years, and was 3 years clear of cancer when his walking became really uncoordinated. He went to the ED in Warrnambool on Monday 5th July and received the news that he had a tumour compressing his spinal cord, therefore affecting his movement. They had also found a lesion on his brain.
He was flown to The Alfred in Melbourne overnight for spinal surgery on the Tuesday.
He recovered from the surgery well, and had rods inserted at his T3 vertebrae to stabilise where they had removed the tumour. The surgeon was pretty confident that they had removed most of it, but had to confirm they had removed enough.

The physio came in the following day to sit dad up on the edge of the bed, which he was able to do but with pain. They were pretty optimistic about his chances of getting back function in his legs. Then the weekend came, and he didn’t see the physio for the next 3 days. In that time he had ‘deconditioned’ to the point that when they tried to sit him up he was ‘like a bag of lose bones’. He wasn’t going to be able to weight bear, let alone walk.
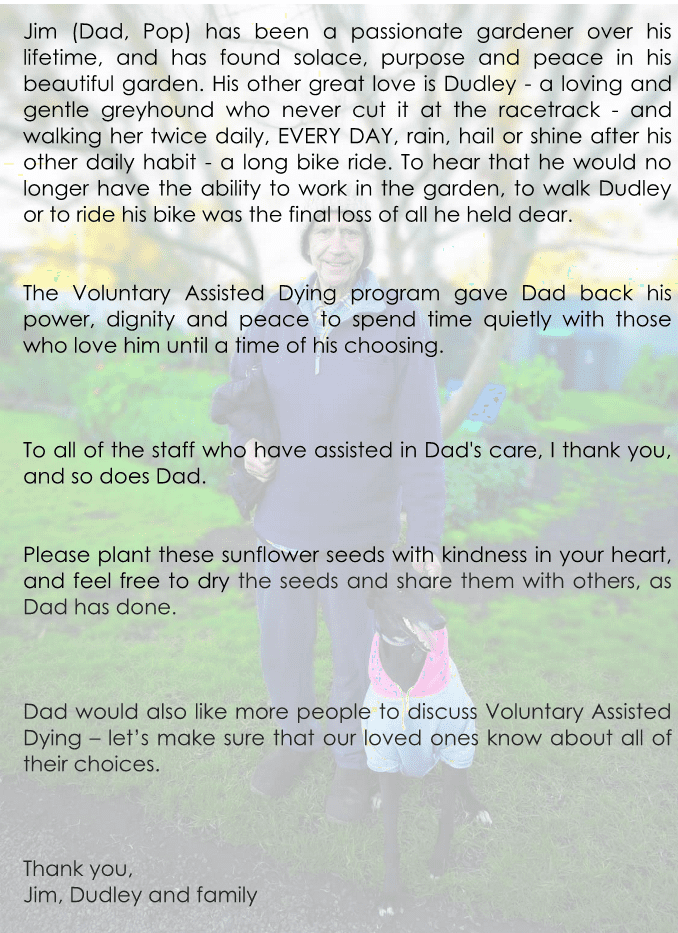
A bit of background for you. Jim was 69 years old, and lived alone in a small country town called Mortlake. He lived a very simple life, and found joy in 3 main things – his garden, walking his rescue greyhound Dudley (a girl, but a ‘dud’ at the race track!) and riding his bike. Dad had a daily routine that never waivered – he would get up at 6am, walk Dudley, then ride 10 km on his bike and spend the rest of the day in his garden. He would then ride another 10 km in the afternoon, then walk Dudley again.
Dad lost his wife – my mother – in 1984, and had become an alcoholic. His laryngeal cancer in 2000 ended his drinking, and all eating as well, as a resulting affect of the cancer surgery was needing a PEG tube for all food and liquid. He moved from SA to Warrnambool, then Mortlake to be nearer to me and my family. Despite being one of three children, I was the main support for Dad, with my younger sister Emily being back up if I needed.
Back to The Alfred…. Dad was a very impatient patient, and got really frustrated really quickly when people didn’t listen to him. The nursing staff on the ward were very young, and not experienced with a PEG tube at all, and the dietician had changed his daily routine of feed times and amounts, causing Dad huge frustration. Dad was a passive person, but aired his frustrations when he needed to. In all, he hated it in Melbourne at the hospital. We found it really difficult to get any information from the doctors about the cancers that they had found. Dad had told the doctors – registrars or interns – that he wanted out. He told them a number of times that if he wasn’t going to be able to get home and walk then he wanted to be ‘put out of his misery’. At no point did any of the medical team request any social work involvement. I found a pamphlet at the nurses station about Advanced Care Planning and Dad and I talked about it, and what his options might be.
In researching the Care Planning I came across a reference to the VAD program, jogging my memory that it had become legal a few years ago. Finally we asked the registrars for more info than they could provide and they requested the surgeon come and speak to us. He was the first person who listened. He told us that the oncology team were still unsure about a prognosis of the cancer, and when Dad said to him “mate, if I treated my dog like this I would be put in jail. Can’t you just put me out of my misery?” he finally understood what Dad was wanting.
He put us in touch with the VAD contact at The Alfred, who came to speak to Dad about what it all meant. After she spoke with Dad she called me to discuss.
I knew that this was what Dad wanted. He was very clear that the only joy he found in his life was in gardening, riding his bike and walking Dudley, and that without those things he had no quality of life. He told me that ‘the perfect thing would be to see a photo of Dudley, go to sleep and never wake up.
We prioritised getting him back to Warrnambool hospital, where we could start the process.
He came back to Warrnambool on Friday 16th July. I took Dudley in to the hospital to see him that day. We met with the VAD and Palliative Care manager on the Friday as well. She brought us information and talked to us about what was involved, and that there was a process of application etc. Dad visibly relaxed as soon as he realised that someone was listening to him, and taking his request seriously. She explained that Dad had to be able to take the medication himself, as there was no option for practitioner assisted dying in Warrnambool. If Dad lost the ability to self administer he would have to be taken to Geelong. She also explained that Dad couldn’t take the medication in hospital, that he would have to be transported home, or to somewhere else for the final step. We agreed that my house would be the best. Dad stated that he was ‘happy to do it in the carpark’, he just wanted it done. At this point we also raised the fact that Dad couldn’t swallow a liquid, as all of his intake was through his PEG tube. This caused a minute of alarm, as the pharmacists had to be consulted to make sure this was possible and within the guidelines.
I took home the information booklet that the VAD person gave us and read through it over and over again. I explained to Dad what it meant, and again reminded him that it was an application and approval process.
As much as it was a really sad time I totally understood that Dad was serious when he said he wanted this – he had fought and fought and fought, been knocked down and gotten up again every time, but this time he was done. The things he was going to lose meant that life would be unbearable for him. My brother and sister also supported Dad in his wish to end his life.
On Saturday morning the VAD person told Dad that she had arranged for the VAD registered doctor – a local GP – to come and see Dad, and we were all surprised to hear that he could come on the Monday. So soon! This was a bit of a shock to me, as even though we had talked about it, and I was happy to support Dad in it, to have the first bit of action happen made it real.
Over the weekend Dad and I made sure that he understood that he had to start the conversation with the doctor, and that he had to make the request. It was quite the rehearsal…
On Monday the doctor came to meet with Dad and I, and straight after being introduced, Dad stated “I wish to take full advantage of the Voluntary Assisted Dying program.” He was going to make damn sure there was no confusion as to what he wanted! The doctor was great, and again went through the process and possible time frames with Dad and I, and he really listened to what Dad said. At the end of it I witnessed something I have never, ever seen in all the years and dealings that Dad has had with doctors. Dad shook the doctors hand and thanked him. Dad is not a fan of the medical profession, thinking most of them are ‘wankers’… I also witnessed another thing I hadn’t seen before – a true look of peacefulness in Dad. His happiness in the fact that someone was listening to him was visible. The biggest surprise for me was when the doctor asked for Dad to treat his involvement with confidentiality. I had no idea that there would be anything other than gratefulness that VAD doctors existed, but to hear that they were targeted absolutely blew me away in disbelief. And to have this also confirmed by the VAD person at the hospital again floored both Dad and I. I was gutted to think that there was opposition to people accessing this choice.
At this point we still hadn’t had any information about the cancer prognosis, so we weren’t sure if Dad would in fact be eligible for VAD. The doctor had explained to us that this would not be a matter of days, that it wouldn’t happen next week, or even the week after so Dad had realistic expectations. He also explained that the next step was gathering further information about his prognosis and booking the assessment with the second doctor.
In this time the medical and nursing staff allowed Dad to take charge of his PEG feeding again (he was very motivated to do this – not only to get back his independence, but also to make sure he was still able to do it himself!), and to have what he wanted at the times that he wanted. The physio and OT staff arranged a reclining wheelchair for Dad to be hoisted into every day. The palliative care doctor made sure that Dad had his usual medication and adequate pain relief. A student doctor working with the palliative care doctor spent time with Dad, asking many questions about Dad’s decision, his medical issues and how he was feeling as a fellow human being. This was a great thing that Dad appreciated – ‘hopefully it makes him a good doctor and not just a wanker’….! And best of all Dudley visited Dad every single day. It often took us a while to get from the door to his room, as everyone we passed wanted a pat and a chat.
I chose not to work in this time. The time that I was able to spend with Dad in this period was something that I will always cherish. Some tough conversations, some funny conversations, some sad conversations and a lot of time with no words, just sitting – me knitting, Dad patting Dudley or just looking outside, sitting with his thoughts.
Finally Dad had his second medical assessment, this time with an oncologist who confirmed that Dad had less than 6 months to live. Somewhat macabrely, Dad and I were overjoyed to hear this news.
I had taken all of Dad’s identification papers to the coordinating doctor, who had commenced the application on the portal. The next step was for Dad to sign his written request with the doctor. This was done with great support from the team, with the VAD person and the student doctor also being present. After discussion, my partner Terry had agreed to be the contact person, as it was a role I didn’t know if I’d be up to on the day. After all of the signing was done, the doctor again shook Dad’s hand, and said to him “well Jim, I’m not sure if I will see you again, but it has been a pleasure meeting you, and I wish you all the best.” This was really hard to hear, but the reality of the situation. Dad again thanked him for listening to him, and also for choosing to be a VAD doctor.
I had noticed a few cards on the ward thanking the staff for caring for loved ones. Dad is not a ‘gift or card’ kind of person, but did want to say thank you. I suggested to Dad that I put some sunflower seeds that he had dried from his garden into envelopes for the staff, and do up a small letter of thanks. He thought it was a great idea. I have attached what we wrote and gave to the staff. On each envelope of seeds I wrote “Jim’s sunflowers. #VADbravechoice”.
Dad’s permit was approved on Monday 2nd August.
Dad was so visibly happy it made any thoughts of personal sadness impossible.
Being the organised person that he was, he wanted to book the day and time straight away, so he did. After confirmation that the pharmacy was able to deliver the medication on Thursday Dad booked in Thursday at 3:30pm. This enabled Dad to contact the people that were important to him to tell them what was happening, and to say his goodbyes. Dad had told me that he ‘didn’t care who came – I don’t care if there are 100 people or none, it’s not my place to ask anyone to be there.’ My sister and brother had spent time with Dad over the preceding weeks, and both wanted to be with Dad at the end. Dad’s very close friend Yan – who had also visited him every day – also wanted to be with Dad.
The hospital arranged for a bed to be delivered to my house the day before – I’d requested a hi-lo bed that lowered all the way to the floor so Dudley could lie down with Dad if she wanted to.
My partner Terry, sister Emily and Dad’s friend Yan all walked Dad home from hospital in his wheelchair at 10am on Thursday – a short walk, and time to feel the wind on his face again. Dad sat in the chair and spent time patting Dudley and chatting with my kids for a couple of hours. The VAD person from the hospital arrived bearing a lovely bunch of flowers – sunflowers : ) She had also brought additional medication for Dad should he need – anti-nausea wafer for before he took the medication, an anti-anxiety medication should he feel that he needed it. We played music and chatted – not always to Dad, he was content to watch and listen and sit with his thoughts.
The pharmacy staff then arrived with the medication. The two men that came were wonderful human beings. They were kind and compassionate, thorough and very open about their commitment to VAD. They spoke with Dad and explained the medication and how it would work. They went through things with Terry and the VAD person and confirmed that they understood what was required.
We had lunch, chatted, laughed, cried, listened to more music and songs that Dad liked and sat with our thoughts. Dad was quick to point out when it was 3:00 – time for the anti-nausea wafer. My brother decided that he didn’t want to be here for the final part, so said his teary goodbyes to Dad and went outside. We helped move Dad from the wheelchair to the bed, and put the bed down to the floor so Dudley could be close to him. At 3:30 Dad was again quick to point out that it was time, so Terry and the VAD person prepared the medication. Dad said his final private words to all of us in turn, told me what songs he wanted to listen to. He also threw in a curveball – a song that he wanted us to listen to after he passed.
Then Terry gave Dad the first syringe – a water flush for his PEG; then the second syringe – the medication that would cause his death; then another syringe of water to flush it down.
Dad lay back on his pillow, patted Dudley, and then after a short time said “I’m getting sleepy now. I love ….. every …… person …………… in this …………………………. room”, yawned, then closed his eyes.
He just looked like he was asleep, and breathing peacefully. After about half an hour he stopped breathing. The doctor arrived shortly after to complete the technical part and officially pronounce Dad as deceased.
Another nurse arrived from the hospital to assist to remove Dad’s catheter and prepare him for the funeral home.
During this entire time Dudley didn’t move from the floor where she lay with Dad – the nurses had to work around her.
And that is our story! Every single interaction we had with any of the VAD staff was positive, informative, non-judgemental, thorough and reassuring. There was not one moment that we felt unsupported, or had questions that went unanswered. My only surprise – and also a surprise for Dad – was how few people know about VAD, and that it is now legal. Even nurses! Many look at you and say ‘is that a thing now? Is that legal?’ Something that became important to Dad was making sure that people know about it, and that it is an actual choice for some people. The other thing we found surprising was the opposition to it, and the fact that medical professionals associated with VAD were targeted and abused.
The staff at South West Healthcare in Warrnambool were amazing – supportive, accommodating and exemplary in all aspects.
After Dad passed away I have made a point of posting things about VAD on Facebook and Instagram, using the hashtag of #VADbravechoice. I will be taking additional seeds, along with Dad’s letter of thanks, to my workplace for staff. I also took the VAD information book that I was given to my work for people to read. Given that my workplace is also the hospital I hope it educates the right people! I’m not out to ‘push a barrow’ or to convince people that it is ‘good’, but I will be telling anyone who will listen about it, so that people at least know that it is a choice. My hope – and Dad’s – is that it will become a topic of conversation, if only to explain where the sunflower seeds came from!

